By the age of eighteen, the average adult has 32 teeth; 16 teeth on the top and 16 teeth on the bottom. Each tooth in the mouth has a specific name and function. The teeth in the front of the mouth (incisors, canine and bicuspid teeth) are ideal for grasping and biting food into smaller pieces. The back teeth or molar teeth are used to grind food up into a consistency suitable for swallowing.
The average mouth is only large enough to accommodate 28 teeth. It can be painful when 32 teeth try to fit in a mouth that can only hold 28 teeth. These four other teeth are your Third Molars, also known as “wisdom teeth.”
Why Should I Remove My Wisdom Teeth?
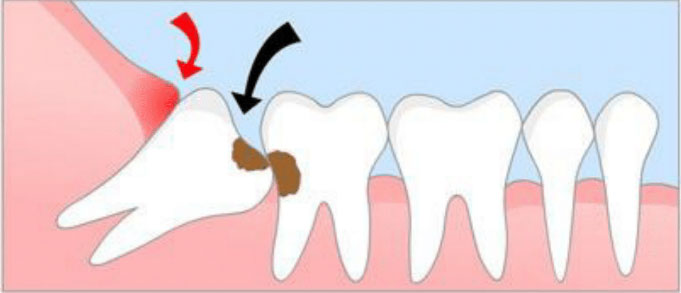
Wisdom teeth are the last teeth to erupt within the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not generally happen. The extraction of wisdom teeth is necessary when they are prevented from properly erupting within the mouth. They may grow sideways, partially emerge from the gum and even remain trapped beneath the gum and bone. Impacted teeth can take many positions in the bone as they attempt to find a pathway that will allow them to erupt successfully.
These poorly positioned impacted teeth can cause many problems. When they are partially erupted, the opening around the tooth allows bacteria to grow and will eventually cause an infection. This results in swelling, stiffness, pain and illness. The pressure from the erupting wisdom tooth may move other teeth and disrupt the orthodontic or natural alignment of teeth. The most serious problem occurs when tumors or cysts form around the impacted wisdom tooth, resulting in the destruction of the jawbone and healthy teeth. Removal of the offending impacted tooth or teeth usually resolves these problems. Early removal is recommended to avoid such future problems and to decrease the surgical risk involved with the procedure.+
Wisdom teeth can be difficult to clean. And in those cases where they are, they are at greater risk of developing periodontal problems (gum disease). As we discuss below, this is an important issue because the gum health of your 3rd molars doesn’t just affect them alone but possibly other teeth in your mouth as well. And for this reason, the removal of your wisdom teeth may be a needed preventive measure.
Oral Examination
With an oral examination and x-rays of the mouth, our doctors evaluate the position of the wisdom teeth and predict if there may be present or future problems. Studies have shown that early evaluation and treatment result in a superior outcome for the patient. Patients are generally first evaluated in the mid- teenage years by their dentist, orthodontist or by an oral and maxillofacial surgeon.
All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. All of our doctors have the training, license and experience to provide various types of anesthesia. At your consult, you and your doctor will select the best type of anesthesia for you.
Removal
In most cases, the removal of wisdom teeth is performed under general anesthesia or local anesthesia and laughing gas. These options as well as the surgical risks (i.e. sensory nerve damage, sinus complications, dry socket) will be discussed with you before the procedure is performed. Once the teeth are removed, the gum is sutured. and gauze is placed in your mouth to bite onto control bleeding. You will rest under our supervision in the office until you are ready to be taken home. Upon discharge, your post-operative kit will include postoperative instructions, a prescription for pain medication and a follow-up appointment.
Our services are provided in an environment of optimum safety and we utilize modern monitoring equipment and medications.
if you decide to undergo wisdom teeth removal, you will be required to read and sign a detailed surgical consent form. This form outlines the potential risks of such a procedure. You can preview this form below.
Why can wisdom teeth be at increased risk for developing periodontal problems?
Gum disease is caused by oral bacteria. And whenever a tooth cannot be cleansed properly on a regular basis, the bacterial-laden film (dental plaque) that accumulates around it may lead to its formation.
The positioning of some wisdom teeth can be such that it makes them exceptionally difficult to clean.
And when this type of added challenge exists, the teeth involved are left at even greater risk for developing periodontal problems.
Challenges unique to wisdom teeth.
Wisdom tooth impaction – In regard to the potential for developing periodontal disease, the worst case situation for a third molar is one where the tooth is locked in a position where it only partially sticks through the gum line (see illustration). When this situation exists, bacteria are able to seep down into the space between the tooth and its gum tissue. The problem is, this area can’t be effectively cleansed and therefore the bacterial colony that develops persists undisturbed.
Gum flaps – Some wisdom teeth have a portion of gum tissue that lies over their chewing surface. This extra tissue is referred to as an operculum.
As you can see in our picture, this extra flap of tissue makes the tooth essentially impossible to access and thoroughly clean, thus placing it at increased risk for developing gum disease.
Difficult access – The general problem that all third molars share is that by nature they occupy a position in the rear of the mouth that is simply difficult to access. That means even non-impacted wisdom teeth can be extremely challenging to keep clean.
When any of the configurations described above exist, the tooth’s risk for developing gum problems (either just minor ones [gingivitis] or advanced [periodontitis]) increases
The gum disease around a tooth is not an isolated event.
For many dental patients the following statements about the need to extract their wisdom teeth may seem a little confusing. It’s common that …
A dentist will suggest removing a wisdom tooth so it doesn’t develop advanced periodontal disease (periodontitis).
But if the tooth isn’t extracted and ultimately does develop gum problems, the treatment recommended at that time is the same, pull it.
With either scenario you end up loosing the tooth. So it’s easy enough to see why a patient would think why not just wait to see if any problems (tooth looseness, pain, swelling) actually occur?
What must be understood is that gum disease isn’t necessarily an isolated event. In fact, it usually isn’t.
Specifically with a wisdom tooth, that region of gum tissue and bone that surrounds its front side is the exact same tissue and bone that supports the backside of the next tooth forward (the 2nd molar).
So, if damage occurs (advanced gum disease [periodontitis] can cause the destruction of bone tissue), two teeth are actually affected not just one
Symptoms and outcome.
This includes both teeth having at least a low-grade chronic infection (the gum disease), becoming loose (as more and more bone is lost), and possibly experiencing an acute infection (with accompanying pain and swelling) from time to time.
Most people would sorely miss a second molar. And it would be a shame to damage or lose one of these valuable teeth simply because a wisdom tooth that could not be cleansed properly was not extracted in time.
Other 2nd molar risks.
It’s not just gum disease that can damage the second molar in this type of situation. Tooth decay may play a role too.
The bone destruction caused by the periodontal disease can leave a deep void that traps food, plaque and debris. This mixture creates the perfect environment for the formation of tooth decay. If it does, the teeth involved may be damaged beyond repair.